The pillar of strength for every family is a Woman. It is no secret that the essence of caring comes from a woman. However, when it comes to the same woman, to start thinking about her own fitness and seek relevant medical advice, the first suggestion that comes to anybody’s mind is, visiting a good Gynaecologist. Many of you might now wonder that what are we doing here talking about Gynaecology when the topic to be understood is Urogynaecology! It will be interesting to begin by knowing the difference between these two terminologies that will help us to understand the problembetter.
Gynaecology and Urogynaecology
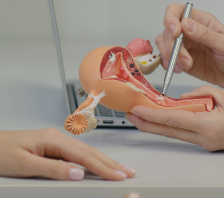
While Gynaecologists attend to women more regularly for common problems, Urogynaecologists are specialists, who receive additional training in Urology and associated part of Gynaecology that helps them to treat women with conditions associated with Pelvic Floor. A good Pelvic health is very important as organs like vagina, uterus, bladder and rectum are supported anatomically and functionally by the pelvic floor.
An insight into Urogynaecology
The common problems for which you will need to visit an Urogynaecologistare with respect to pelvic floor and urinary incontinence. Possible symptoms include the following.
- An overactive bladder leading to frequent visits to the washroom and leakage before reaching the toilet.
- Leakage of urine on daily activities like coughing, sneezing and exercises.
- Losing control over the bladder and feeling a need to urinate (when you otherwise actually wouldn’t want to) with repeated wetting of undergarments.
- Recurrent or Chronic Urinary Tract Infection
- Chronic constipation and bowel problems
- Feeling a bit of pressure, pain in the pelvis
- Feeling a sense of fullness, heaviness, pricking or pulling in the vagina, which increases by the end of the day
- Pain during intercourse, decreased sexual desire
On developing any of the above symptoms, there is no need to feel embarrassed or unduly worried as a qualified Urogynaecologist can comfortably and safely address these issues. It’s just about feeling comfortable in discussing the specific symptoms with your doctors and this is where NU Hospitals, one of the most preferred and recommended hospitals in Bangalore, comes to the picture. NU Hospitals is well known as one of the leading Urogynaecology centre for women and is well equipped with some of the best Urogynaecology doctors, capable of delivering the most advanced treatment, using modern day technology.
It will benefit immensely by understanding some of the common conditions associated with Urogynaecology, which can make your discussion with your Urogynaecology specialist, more comfortable and productive.
What are the common conditions observed in Urogynaecology?
Let’s take a closer look at some of the commonly noticed conditions among patients in Urogynaecology and understand them better.
- Stress and Urge Urinary Incontinence
- Pelvic Organ Prolapse
- Genitourinary Fistula
- Vulvodynia and Pelvic Pain
- Obstetric and Sphincter injuries (OASIS)
- Urogynaecology Procedures
Stress and Urge Urinary Incontinence
In simple terms, unintentional leakage of urine (either in large quantity or few drops), is referred to as Urinary Incontinence. There are two main types of incontinence; Stress Incontinence and Urge Incontinence.
- Stress Incontinence Stress incontinence is a condition that results in leakage of urine when the abdominal pressure is higher than the Sphincter pressure (Sphincter is a muscle that closes the bladder outlet). It can happen due to common physical activity like coughing, sneezing or laughing or either during jumping or walking too. Pelvic floor muscle exercises are the initial and most effective ways to treat stress urinary incontinence. Your doctors might also recommend a stress incontinence surgery, depending upon the severity of incontinence. Studies have also indicated that the success rate for stress continence surgeries is as high as 90%.
- Urge Incontinence This is a condition which occurs due to an overactive bladder that leads to an uncontrollable need to void urine. You leak urine before you decide and reach the toilet. Reducing the consumption of irritants like alcohol, tea or coffee can also play a major role in controlling urge incontinence.
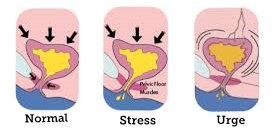
Studies and Researches conducted have also indicated that out of 35-45% of women, who face incontinence problem, about 20-25% are purely stress Incontinence while around 3-5% are purely urge incontinence. The remaining 11% of women are also known to face another condition known as mixed incontinence, which is a mix of both stress and urge incontinence
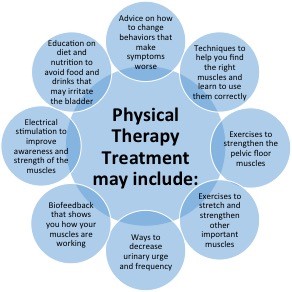
NU Hospitals offers some of the most advanced urinary incontinence treatment options in Bangalore. The types of incontinence treatments include physical therapies, behavioural therapies as well as surgeries.
Pelvic Organ Prolapse
This condition occurs due to weakness in the Pelvic floor muscles. Pelvic organ Prolapse is also referred to as Genital Prolapse or Uterine Prolapse. Prolapse in simple terms means vital organs falling off their original places. Pelvic organ prolapse is a common condition among women with atleast 40% of them facing it at some stage in their lives.
The most common types of Pelvic Organ Prolapse noticed are,
- Cystocele ( Prolapse of Bladder into the Vagina)
- Rectocele (Rectum Prolapse)
- Uterine Prolapse
- Urethrocele ( Prolapse of the Urethra)
- Vaginal Vault Prolapse ( Prolapse of the Vagina)
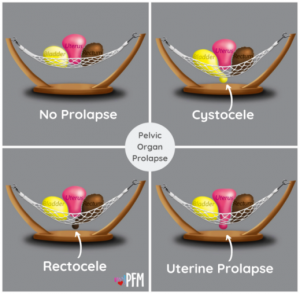
With the advancements in medical science and technology playing a big role, NU Hospitals in Bangalore, has all the required facilities in place which include a team of most competent doctors to offer safe and secure surgical treatment for Uterovaginalprolapse.
Genitourinary Fistula
Fistula is an abnormal connection that might occur between two organs due to either a surgery or injury. Vesicovaginal Fistula is commonly observed among women. They are also referred to as Obstetric Fistulas, which normally occur as the woman’s vagina is abnormally connected to the urinary bladder.The symptoms for Vesicovaginal Fistula generally include leakage of urine through the vagina or an abscess (Build-up of pus within the tissue in the body). Similar fistulas can also exist between uterus and bladder (Vesicouterine fistula),ureter and vagina (Ureterovaginal fistula). Certain imaging tests and evaluations are recommended by doctors to find out the exact cause and suggest relevant treatment.
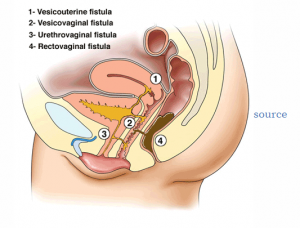
Usually Doctors recommend surgery as the most suitable fistula treatment, since these take a while to heal. These fistulas can even recur if proper pre and post-operative instructions are not followed. This is where NU Hospitals scores overs rest of the available resourcesas the best hospital forgenitourinary fistula treatment in Bangalore. The Hospital continues to educate people about the ailment so that they can understand the problem better rather than blindly believing what the doctors say.
Pelvic Floor and Voiding Dysfunction
Pelvic Floor Dysfunction is the inability to correctly contract (tighten) and relax the muscles in the pelvic floor. Atleast 1 in 4 women suffer from pelvic floor disorder. It is more common than we think. The common causes are multiple and early age of childbirth, traumatic injury to the pelvic region, obesity, pelvic surgery, nerve damage, habit of holding urine for long duration, chronic hard stools. Your doctors might recommend certain tests and examinations to find out the magnitude and complexity involved in the symptoms, to diagnose Pelvic Floor Dysfunction.
Pelvic Floor Dysfunction can often be treated without surgery. Some of the common types of treatments suggested could range from Biofeedback (done by Physiotherapists), medications and by using relaxation techniques which includes yoga and exercises. However, if your doctor finds out the reason for your problem is actually due to urethral stenosis or narrowing, the best option recommended then is, a Buccal Mucosa Graft Urethroplasty.
Vulvodynia and Pelvic Pain
Vulvodynia, to put in simple terms, is a chronic discomfort faced by women in the vulvar region. More often, this pain surfaces without any identified cause. However, the location and intensity of the pain might vary with different patients. Vulvodynia is generally categorized into two types, Localized Vulvodynia, where women experience pain in only one vulvular site and Generalized Vulvodynia where the pain experienced is more constant and spontaneous.
NU Hospitals in Bangalore has been one of the centres which continue to offer high quality treatment with the best team of competent Vulvodynia specialists.
Obstetric and Sphincter injuries (OASIS)
Obstetric and Sphincter Injury is mostly caused due to trauma experienced during vaginal delivery. Commonly noticed symptoms among women for Obstetric and Sphincter Injuries are pain and faecal / Urinary Incontinence. In certain cases, women may also experience sexual dysfunction.
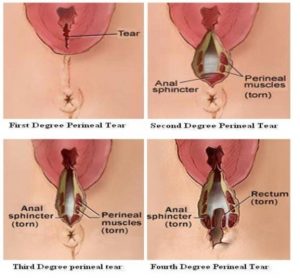
On examination, your doctors might recommend tight sphincter muscle treatments if he notices faecal incontinence or leakage of faeces. Regular treatments can help overcome this problem and strengthen the sphincter muscles. These exercises that focus exclusively on sphincter muscle damage and treatment can also help in improving bowel control. You may need even a sphincter repair as a last resort.
Urogynaecology Procedures
Based on the complexity of the problem your doctors might recommend a surgery. Urogynaecology surgery procedures differ with different types of complaints presented. Some of the common surgical procedures performed are;
- Surgery for Uterovaginal Prolapse: Laparoscopic or open sacrocolpopexy, Vaginal Hysterectomy, Fothergill’s Operation, Cystocele (bladder prolapse) repair, Rectocele (Rectum prolapse) repair, Uterosacral ligament fixation.
- Surgery for vaginal vault prolapse (Post Hysterectomy): Uterosacral ligament fixation, sacrospinous fixation, McCall’s Culdoplasty.
- Surgery for Stress Urinary Incontinence: Tension free Vaginal tape (TOT and TVT), Autologous fascial slings, Urethral Injections.
- Surgery for Urge Incontinence and Voiding dysfunction:Botulinum toxin Injections to urethra and bladder, Botulinum Injection to the tender points in the pelvic floor, Buccal Mucosa Graft Urethroplasty.
- Surgery for Genitourinary fistulas: Transabdominal and Transvaginal repairs, Martius flap interposition, O’Connor VVF repair.
- Surgery for OASIS: Anal sphincter reconstruction, OASIS repairs.
Conclusion
The last decade has seen a rapid advance, in the management options for Urogynaecologists, in treating Pelvic Floor Disorders. Symptoms associated with Urogynaecology are not life threatening, but they can have an impact of the quality of life, faced by women. The need of the hour is the availability of an Urogynaec centre for women,which can implement the most appropriate route of investigation and management.
This is where NU Hospitals makes a difference as a centre par excellence for Urogynaecology. With one of the finest team of best Urogynaecology doctors, ready to handle your medical issues with passion and care, you are absolutely in safe hands. NU Hospitals makes use of niche technology in its treatments across various specialities and hence reaffirms itself as the go to hospital for all your specific needs which require a specialist Urogynaecologist.